Introduction
Infertility affects millions of couples worldwide, making conception difficult or impossible through natural means. In Vitro Fertilization (IVF) has revolutionized reproductive medicine, offering hope to those struggling with infertility. Since the birth of the first “test-tube baby,” Louise Brown, in 1978, IVF has helped millions of families achieve pregnancy. This article explores how IVF works, its success rates, benefits, risks, and ethical considerations.
What Is IVF?
IVF is an assisted reproductive technology (ART) where fertilization occurs outside the body. Eggs are retrieved from the ovaries and combined with sperm in a laboratory. The resulting embryos are monitored and then transferred into the uterus to establish a pregnancy.
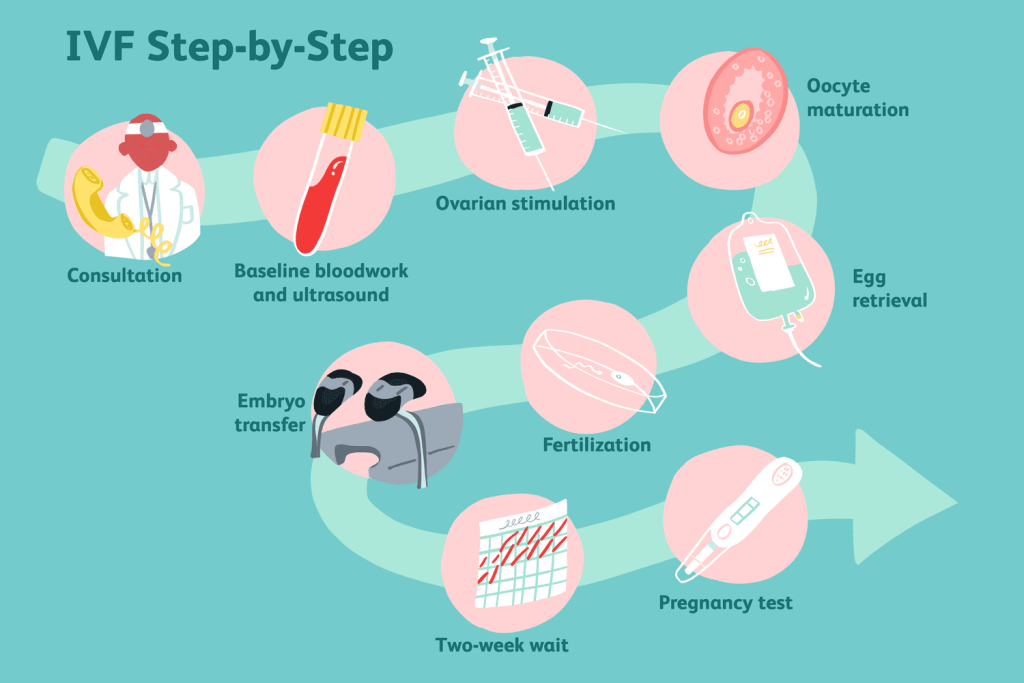
The IVF Process Step-by-Step
- Ovarian Stimulation
- Fertility drugs are used to stimulate the ovaries to produce multiple eggs.
- Regular ultrasounds and blood tests monitor hormone levels.
- Egg Retrieval
- A minor surgical procedure extracts mature eggs from the ovaries.
- Performed under sedation, taking about 20-30 minutes.
- Sperm Collection
- A semen sample is collected (from a partner or donor).
- Sperm is processed to select the healthiest for fertilization.
- Fertilization (In Lab)
- Eggs and sperm are combined in a petri dish (conventional IVF).
- Alternatively, Intracytoplasmic Sperm Injection (ICSI) may be used, where a single sperm is injected directly into an egg.
- Embryo Development
- Fertilized eggs (embryos) are cultured for 3-5 days.
- The best-quality embryos are selected for transfer.
- Embryo Transfer
- One or more embryos are placed into the uterus using a thin catheter.
- Excess viable embryos may be frozen (cryopreserved) for future use.
- Pregnancy Test
- A blood test is conducted about 10-14 days after transfer to confirm pregnancy.
Who Can Benefit from IVF?
IVF may be recommended for:
- Women with blocked or damaged fallopian tubes.
- Couples with male infertility (low sperm count/motility).
- Individuals with ovulation disorders (e.g., PCOS).
- Same-sex couples or single parents seeking biological children.
- Those with genetic disorders (using Preimplantation Genetic Testing, PGT).
Success Rates and Factors Affecting IVF
- Age is the most critical factor—women under 35 have a higher success rate (~40-50% per cycle).
- Ovarian reserve, sperm quality, and uterine health also impact outcomes.
- Multiple cycles may be needed for success.
Risks and Challenges
- Multiple pregnancies (if more than one embryo is transferred).
- Ovarian Hyperstimulation Syndrome (OHSS) (rare but serious).
- Ectopic pregnancy (embryo implants outside the uterus).
- Emotional and financial stress (IVF can be costly and emotionally taxing).
Ethical and Social Considerations
- Embryo selection & genetic screening (PGT raises ethical debates).
- Surrogacy and donor eggs/sperm (legal regulations vary by country).
- Frozen embryo dilemmas (choices regarding unused embryos).
Conclusion
IVF has transformed reproductive medicine, offering hope to countless individuals and couples. While it presents challenges—medical, financial, and ethical—advancements in technology continue to improve success rates and accessibility. Consulting a fertility specialist is essential to determine if IVF is the right path toward parenthood.



